What is it like to have Keratoconus?
To say the eye is a sophisticated organ is an understatement. That complexity allows humans to see but also creates a wide range of circumstances that can impair your vision. Understanding these diseases and their treatments is critical for determining whether to consult with one of our Fort Lauderdale eye doctors. Keratoconus is one such disorder that affects the shape of the eye’s cornea and has long-term effects on a patient’s eyesight quality.
What exactly is Keratoconus?
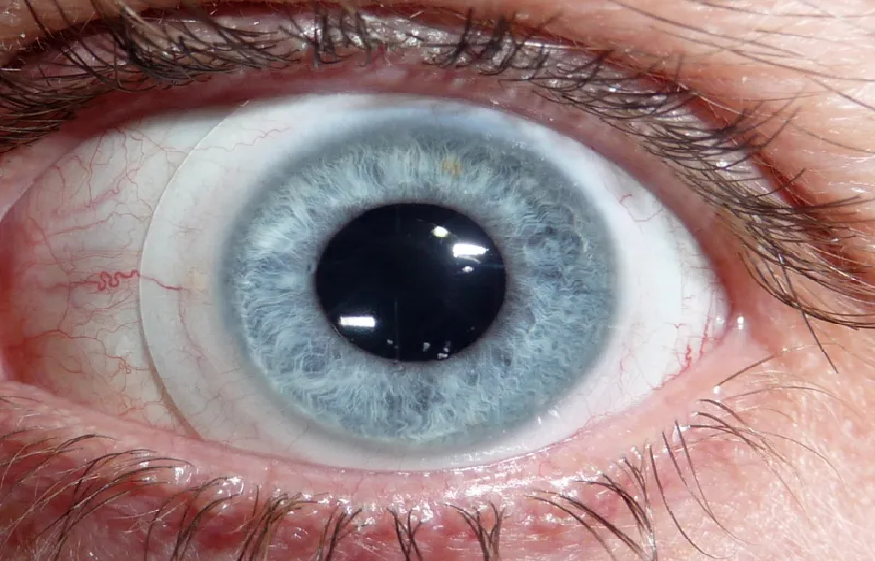
The cornea, the most outer layer of the eye, is your eye’s first line of protection and a vital role in focusing light into your pupil and eventually onto the retina. Unfortunately, in a keratoconus patient, the cornea weakens and thins, eventually becoming too fragile to maintain its semi-spherical form in the eye. As a result, the cornea’s shape gradually changes. This progressive alteration usually affects both eyes, albeit asymmetrically.
These alterations gradually reshape the cornea into a cone-like shape, lending the illness its name. Keratoconus patients frequently report near-sightedness, fuzzy vision, distorted pictures, and excessive glare when viewing lights, particularly at night. Although the illness is usually not unpleasant, it can significantly influence a person’s visual acuity.
Typical Keratoconus Treatment Options
RGP lenses were once thought to slow the advancement of Keratoconus, but we now know this is not the case. RGP lenses can be uncomfortable and annoying for people who have Keratoconus. Scleral lenses, on the other hand, are a better option. Instead of resting directly on the cornea, these lenses vault the cornea and place all of their weight on the sclera, or “white of the eye.” As a result, scleral lenses achieve superior comfort while providing exceptional stability and the visual benefits patients need by avoiding real contact with the cornea.
While scleral lenses can help with vision improvement, they are not a “cure” for Keratoconus; they are a better and more comfortable choice for correcting vision with this condition. However, it is possible to delay the course of Keratoconus and reinforce the cornea to avoid additional long-term abnormalities. Corneal collagen crosslinking, or CXL is a simple in-office technique involving vitamin B2 drops. UV light activates the solution and causes natural collagen fibres in the cornea to re-link and strengthen. Until CXL may improve eyesight in some patients, scleral lenses remain the best long-term therapy option while CXL prevents its progression.


